Dr Erin Louise Bellamy founded Integrative Ketogenic Research and Therapies which uses principles of Metabolic Psychiatry to provide remote, highly personalized 1:1 Metabolic Therapy for both psychiatric conditions and overall metabolic health.
Dr. Erin Bellamy has a PhD in Psychology, specializing in Ketogenic Diets & Depression from the University of East London. She also has an MSc in Psychiatric Research from the Institute of Psychiatry at King’s College London. She is a Chartered Psychologist, an Associate Fellow of the British Psychological Society and an accredited member of the Society of Metabolic Health Practitioners.
In this episode, Drs. Brian and Erin talk about…
(00:00) Intro
(01:36) How Dr. Erin became interested in Metabolic Psychiatry
(05:38) Ketogenic diets and psychiatric conditions
(15:39) Fasting and mental clarity
(18:12) The areas in which clinical psychology is deficient in helping patients
(23:46) Adverse childhood events, PTSD, and metabolic health
(28:24) Binge eating, stress, and support groups
(40:00) Food addiction and ketosis
(43:59) Schizophrenia, autism, and ketosis
(01:00:46) Outro/plugs
summerizer
Summary
This episode of the Low Carb MD podcast features Dr. Erin Bellamy, a psychologist and metabolic health practitioner (MHP), who shares her compelling journey into metabolic psychiatry—the emerging field that addresses mental health through metabolic and nutritional interventions such as ketogenic diets. Dr. Bellamy recounts her early experiences working on psychiatric inpatient wards and her research path, which revealed striking historic and modern evidence showing profound mental health improvements linked to low-carbohydrate and ketogenic therapies.
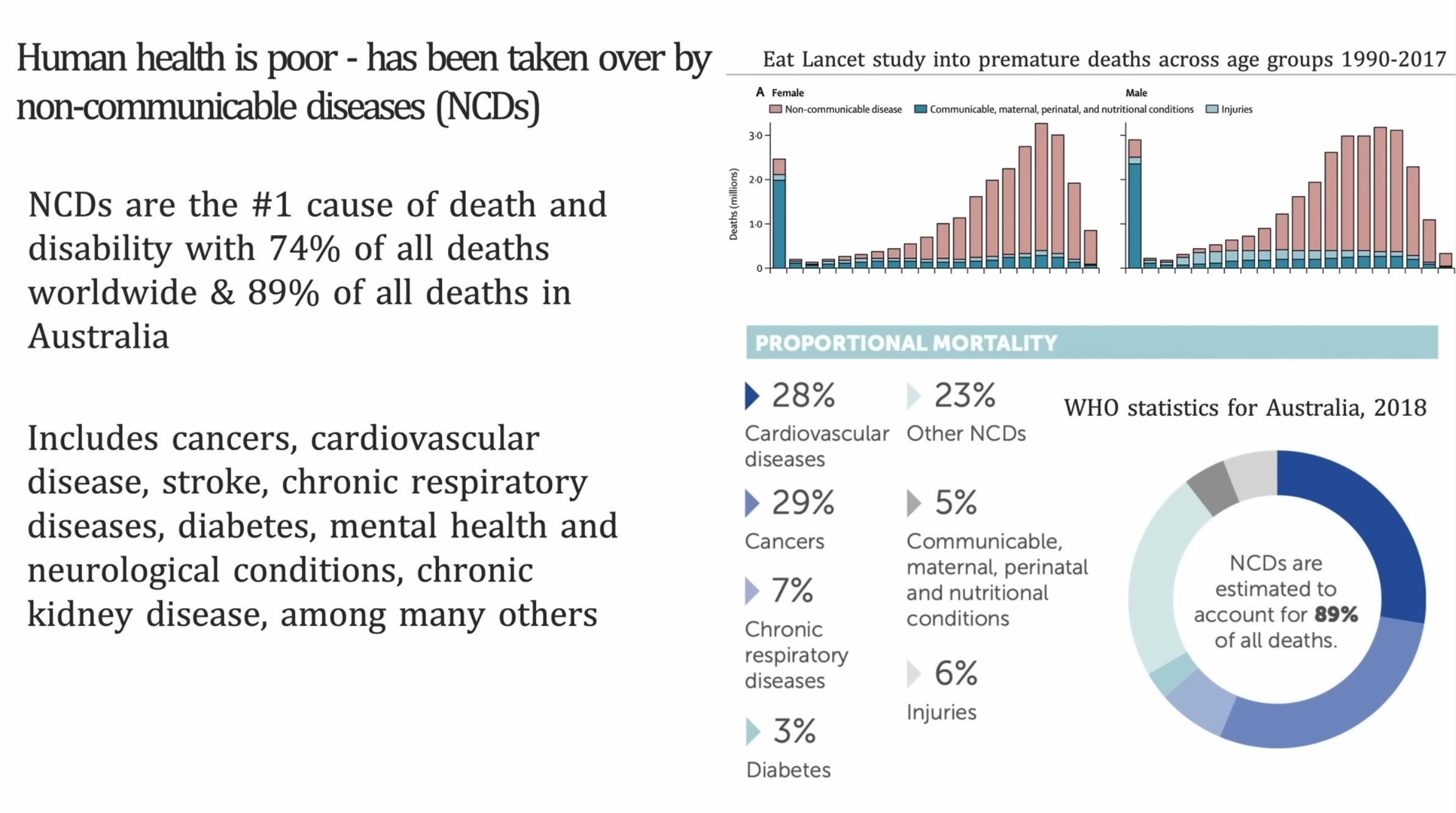
The conversation highlights the strong interconnection between metabolic health and mental health, emphasizing how metabolic dysregulation, particularly in conditions like diabetes and schizophrenia, can directly impact mood, cognition, and psychiatric symptoms. Dr. Bellamy stresses the importance of a multidisciplinary approach, combining nutrition, sleep, light exposure, exercise, and psychological support to build resilience against mental illness.
The podcast also addresses systemic challenges in mental health care such as medication-centric models, long wait times for psychiatric care, and the lack of holistic lifestyle integration. Dr. Bellamy explains her group programs designed to educate and support people with various psychiatric diagnoses through ketogenic metabolic therapy, fostering community and sustained lifestyle change. Throughout, hope and empowerment surface as central themes, underscoring that with appropriate metabolic care and social support, even treatment-resistant symptoms can improve dramatically.
Highlights
- 🧠 Metabolic health is a foundational pillar for improving mental health conditions such as schizophrenia, bipolar disorder, and depression.
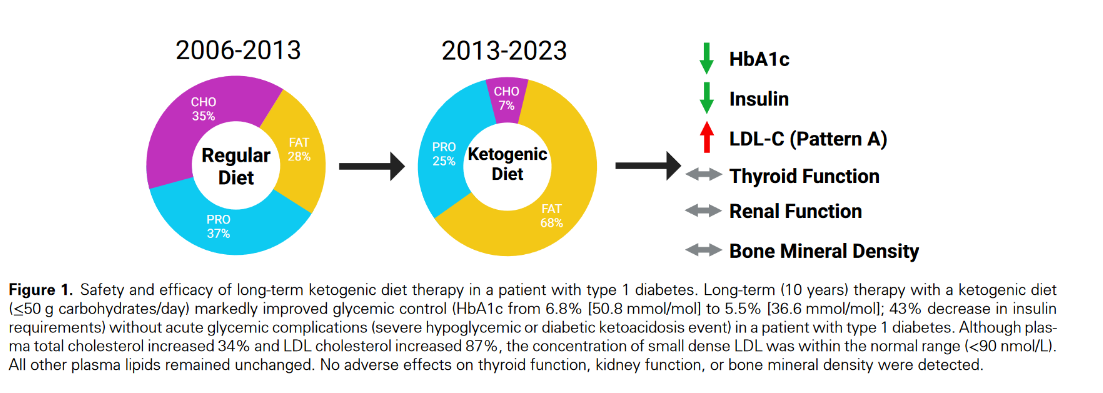
- 🍳 Ketogenic diets historically and currently show promising results in alleviating severe psychiatric symptoms.
- ⏳ There is a disturbing research gap between early studies (1960s) and modern psychiatry overlooking nutrition’s role in mental health.
- 👥 Group support and community involvement significantly increase adherence and success in metabolic psychiatry interventions.
- 🚀 Multidisciplinary collaboration including psychologists, psychiatrists, and metabolic health practitioners is critical for integrated care.
- 🔄 Metabolic psychiatry offers hope for treatment-resistant mental illness by addressing root metabolic dysfunctions.
- 🌱 A holistic pyramid approach with nutrition as the base, supplemented by sleep, stress management, exercise, and social connection is vital. Key Insights
🧬 The metabolic basis of mental illness is historically recognized yet underappreciated: Dr. Bellamy points to early research from as far back as 1930s and a pivotal 1965 study showing ketogenic diets improving schizophrenia symptoms. This suggests a biological underpinning of mental disorders linked to metabolic processes, which modern psychiatry has largely sidelined in favor of drug-centric interventions.
🔄 Metabolic dysregulation precedes and exacerbates psychiatric symptoms: The discussion reveals that poor blood sugar control and insulin resistance can precipitate depression and anxiety rather than these mental illnesses being purely psychological or behavioral in origin. This shifts the treatment paradigm toward addressing metabolic imbalances as causal factors.
🤝 Holistic, multi-layered care improves outcomes: Dr. Bellamy’s “metabolic pyramid” model prioritizes nutrition as the foundation, with layers including sleep optimization, light exposure, exercise, stress reduction, and social connection. This comprehensive strategy recognizes that sustainable mental health improvements require addressing environmental, lifestyle, and biochemical factors simultaneously.
💬 Social and clinical support enhances adherence: Ketogenic and metabolic therapies demand significant lifestyle changes, which are difficult without structured support. The podcast underscores the critical role of group programs, peer accountability, and integration into multidisciplinary teams to maintain motivation and long-term success, especially in complex psychiatric populations.
🔍 Current mental health systems inadequately address metabolic health: Patients face long waits for psychiatric care focused narrowly on medications with debilitating side effects that worsen metabolic health. Psychologists are positioned to bridge the gap but are often disconnected from nutritional interventions. A reframing toward metabolic psychiatry could transform treatment protocols.
🌿 Hope and patient empowerment are therapeutic: Offering patients a tangible, active role in managing their health through ketogenic metabolic therapy fosters agency and reduces feelings of helplessness common in chronic mental illness. The ability to control symptoms through diet and lifestyle has profound psychological benefits beyond physiology alone.
⚖️ Flexibility and balance are key: Successful programs encourage realistic planning, allowing occasional social indulgences without guilt, emphasizing control and balance rather than strict deprivation. This practical approach supports mental wellbeing and reduces relapse driven by shame or all-or-nothing mindsets.
This episode illuminates how revisiting and integrating metabolic science into mental health care offers groundbreaking potential for improving lives devastated by psychiatric illness. Dr. Bellamy’s experience and research-based optimism call for a paradigm shift to holistic, metabolism-centered psychiatry supported by community and clinical collaboration.