Low Carb High Fat - Ketogenic
A casual community to talk about LCHF/Ketogenic lifestyles, issues, benefits, difficulties, recipes, foods.
The more science focused sister community is [email protected]
Rules
- Be nice
- Stay on topic
- Don’t farm rage
- Be respectful of other diets, choices, lifestyles!!!
- No Blanket down voting - If you only come to this community to downvote its the wrong community for you
In this presentation, Dr. Matthew Budoff reveals preliminary results from Heartflow’s AI-guided quantitative analysis of the Keto-CTA study. The data focus on coronary plaque progression in participants adhering to a ketogenic diet who experienced a significant rise in LDL cholesterol. Budoff compares the Heartflow data to previously released analyses, discussing patterns of regression, progression, and distribution across key subgroups. This early analysis supports the plausibility and biological consistency expected in longitudinal CCTA imaging, particularly among those with low baseline plaque burden.
Note: Heartflow was unable to process 5 of the 200 scans due to technical limitations. These participants are excluded from all quantitative analyses in this presentation to ensure consistent comparison across datasets.
summerizer
Summary
Dr. Matthew Budoff, a professor of medicine at UCLA School of Medicine, presented findings from the Keto Trial, a prospective study investigating the effects of carbohydrate-restricted ketogenic diets on LDL cholesterol elevation and coronary plaque progression in a specific subgroup called "lean mass hyperresponders." These individuals, despite being metabolically healthy and lean, experience significant LDL cholesterol increases (greater than 190 mg/dL) when on a ketogenic diet. The study enrolled 100 participants who strictly adhered to a ketogenic diet (<30 grams of carbohydrates per day) for one year, with rigorous cardiac CT angiography imaging at baseline and follow-up to assess coronary plaque changes.
The trial focused primarily on changes in total non-calcified coronary plaque volume and secondary changes in low attenuation plaque (LAP), which is associated with vulnerable plaque and higher cardiovascular risk. Multiple analytic tools were employed, including semi-quantitative total plaque score assessments, Clearly software analysis, and advanced AI-based HeartFlow plaque quantification validated against the invasive gold standard intravascular ultrasound (IVUS).
Results demonstrated that about 40-50% of participants showed plaque progression, while 50-60% showed no change or even regression, depending on the measurement method. The HeartFlow AI tool and blinded total plaque scores were consistent, revealing some regression in a minority of patients, whereas the Clearly software indicated nearly universal progression, showing discordance with the other methods.
Importantly, low attenuation plaque was rare and did not significantly increase over the year, suggesting limited development of vulnerable plaque in this cohort despite elevated LDL. Patients with zero baseline coronary calcium scores (calcium score of zero) generally showed minimal or no progression, consistent with prior studies that identify zero calcium as a strong predictor of low risk.
The findings suggest that while LDL cholesterol rises dramatically in lean mass hyperresponders on ketogenic diets, this does not universally translate into rapid or extensive coronary plaque progression within one year. Some individuals even exhibited plaque regression, and vulnerable plaque remained uncommon. Further detailed analyses using the Medis Qangio software are pending, with final results expected in 2025.
Highlights
- 🥑 Ketogenic diet induces significant LDL cholesterol elevation in lean mass hyperresponders.
- 🫀 100 metabolically healthy patients followed for one year with cardiac CT imaging.
- 💻 HeartFlow AI plaque quantification validated by invasive intravascular ultrasound, showing high accuracy.
- 📊 About 40-50% showed plaque progression; 50-60% had no change or regression depending on measurement method.
- 🔵 Low attenuation plaque (vulnerable plaque) was rare and did not increase significantly.
- 🧮 Patients with zero baseline coronary calcium score had minimal plaque progression.
- 🔍 Discordant results between Clearly software and other plaque assessment tools highlight methodological challenges.
Key Insights
-
🩺 Lean mass hyperresponders show significant LDL increases but heterogeneous plaque responses: Despite LDL cholesterol levels rising to an average of 272 mg/dL, only a subset of patients showed measurable coronary plaque progression. This challenges the simplistic notion that elevated LDL universally accelerates atherosclerosis in the short term, especially in metabolically healthy individuals. It underscores the complexity of cardiovascular risk beyond lipid levels alone.
-
🤖 AI-based HeartFlow plaque analysis correlates strongly with invasive gold standards: The HeartFlow software demonstrated excellent concordance with intravascular ultrasound (IVUS), affirming its utility as a reliable non-invasive tool for quantifying coronary plaque volume and composition. This technology represents a significant advance in cardiovascular imaging and risk stratification, enabling more precise monitoring of plaque changes over time.
-
⚠️ Low attenuation plaque remains uncommon despite high LDL: Vulnerable plaque, characterized by low attenuation on CT and associated with higher risk of cardiovascular events, was infrequent and stable in this cohort. This is clinically reassuring and suggests that short-term LDL elevation induced by ketogenic diets may not immediately promote the formation of high-risk plaque phenotypes, at least in the absence of other metabolic dysfunction.
-
📉 Plaque regression occurs in some patients, indicating potential protective mechanisms or variability in plaque biology: Approximately 6% of patients demonstrated plaque regression, confirmed by both HeartFlow and blinded semi-quantitative scoring. This finding highlights heterogeneity in individual responses to diet-induced lipid changes and raises questions about the role of diet, inflammation, genetics, and other modulators in plaque dynamics.
-
💡 Baseline coronary calcium score remains a powerful predictor of plaque progression: Patients with a zero calcium score at baseline tended to have little to no plaque progression or even slight regression, while those with positive calcium scores had more plaque progression. This aligns with established literature emphasizing the prognostic value of coronary calcium as a marker of atherosclerotic burden and risk.
-
🔄 Discordance among plaque assessment tools underscores the importance of method selection: The Clearly software indicated nearly universal plaque progression, contradicting HeartFlow and blinded scoring results. This discrepancy highlights challenges in plaque quantification methodologies, the need for standardized assessment tools, and cautious interpretation of AI-driven outputs without validation.
-
🔮 Long-term implications of diet-induced LDL elevation require further study: While one year of ketogenic diet-induced LDL elevation showed mild plaque progression, the absence of significant vulnerable plaque growth provides some reassurance. However, longer follow-up is essential to understand if these changes translate into clinical events or accelerated atherosclerosis over time, particularly as the ketogenic diet gains popularity.
Conclusion
The Keto Trial provides a nuanced view of cardiovascular effects in lean mass hyperresponders on ketogenic diets, revealing that dramatic LDL cholesterol elevations do not necessarily equate to widespread or rapid coronary plaque progression within a year. Advanced imaging techniques, especially AI-validated HeartFlow analysis, offer detailed and reliable insights into plaque biology, identifying both progression and regression patterns. The rarity of vulnerable plaque and the protective profile of zero calcium score patients add important clinical context to interpreting lipid elevations in this setting. This study advances the understanding of diet-induced lipid changes and their impact on coronary artery disease risk, while emphasizing the need for ongoing research and individualized cardiovascular risk assessment.

Hangry - Or Anger when Hungry - Isn't normal.
It's a sign of insulin resistance.
Small hypoglycemic dips can cans irritability, cortisol increases, and "hangry-episodes". hence the commercial tag line "You're not you when your hungry".
There are two major causes of insulin resistence
- Persistently elevated glucose levels
i.e. Eating carbohydrate rich meals, and carbohydrate meals throughout the day.
- Industrial Oil consumption / Seed Oils / Vegetable Oils
A much cheaper fat source only available in modern day these oils have high levels of Linoleic Acid which interferes with cell mitochondria reducing energy production in cells as well as creating inflammation. Sadly LA can be incorporated into stored fat cells so even between meals the fat the body would normally burn is causing inflammation, and elevated glucose levels.
There are more niche causes, but they are not very common.
What can you do to prevent Hangry episodes?
Improve your metabolic health
- avoid industrial oils in meals when you can (every meal counts).
- reduce fructose consumption (no sweet drinks)
- reduce sugar consumption
- avoid empty carbohydrates
- Buy your food from the edges of the grocery store
- Only buy single ingredient foods (whole foods)
- Meal prep and cook at home for better control
You don't have to go full keto, any small improvement is a victory.
Adhering to the ketogenic diet can reduce or stop seizures, even when other treatments fail, via mechanism(s) distinct from other available therapies. These results have led to interest in the diet for treating conditions such as Alzheimer’s disease, depression and schizophrenia. Evidence points to the neuromodulator adenosine as a key mechanism underlying therapeutic benefits of a ketogenic diet. Adenosine represents a unique and direct link among cell energy, neuronal activity, and gene expression, and adenosine receptors form functional heteromers with dopamine receptors. The importance of the dopaminergic system is established in addiction, as are the challenges of modulating the dopamine system directly. A mediator that could antagonize dopamine’s effects would be useful, and adenosine is such a mediator due to its function and location. Studies report that the ketogenic diet improves cognition, sociability, and perseverative behaviors, and might improve depression. Many of the translational opportunities based on the ketogenic diet/adenosine link have come to the fore, including addiction, autism spectrum disorder, painful conditions, and a range of hyperdopaminergic disorders.
Full Paper At: https://doi.org/10.3389/fnut.2025.1492306

Can adenosine and a ketogenic diet help treat addiction? New research explores the powerful role of adenosine, dopamine, and metabolic health in addiction, and how dietary strategies could support recovery.
In this interview, Dr. Bret Scher speaks with Dr. Susan Masino, a neuroscience and psychology professor at Trinity College, about her groundbreaking work on adenosine and its potential to regulate addiction through metabolic pathways. They dive into:
- The dopamine-addiction connection
- The role of adenosine in addiction and how it balances dopamine activity
- The role of ketogenic diets in boosting adenosine
- Other mechanisms supporting keto for treating addiction
- Why food, sugar, and even phone addiction may share common roots
- How metabolic therapies could support recovery from addiction, depression, and more
Dr. Masino also shares insights on how habits, stress, inflammation, and neuroplasticity all intersect with metabolic health—and what that means for mental health and addiction treatment going forward.
Resources Mentioned: Ketogenic diet, adenosine, and dopamine in addiction and psychiatry - frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1492306/full
summerizer
Summary
The video features an in-depth interview with Dr. Susan Msino, a distinguished professor specializing in applied sciences, neuroscience, and psychology at Trinity College. The conversation explores the intriguing connections between ketogenic diets, adenosine, dopamine, and addiction. Dr. Msino outlines how diet, particularly ketogenic and low-carb diets, may influence addiction behaviors by modulating brain chemistry, specifically through adenosine’s interaction with dopamine. Dopamine, a neurotransmitter linked to reward and habit formation, plays a central role in addiction, but adenosine acts as a natural brake on dopamine activity. This interaction suggests that enhancing adenosine signaling via ketogenic diets could potentially mitigate addictive behaviors and improve metabolic health.
Dr. Msino elaborates on adenosine’s multifaceted role in the brain and body, highlighting its neuroprotective properties, ability to promote sleep, relieve pain, and regulate neuronal metabolism and epigenetics. She explains how adenosine’s receptor activity counterbalances dopamine spikes that lead to addictive cravings. The ketogenic diet is proposed to increase ATP (adenosine triphosphate) production, which is a precursor to adenosine, thereby potentially boosting adenosine’s beneficial effects. This metabolic shift could help reduce addiction risks, improve sleep, and address psychiatric comorbidities such as depression and bipolar disorder.
Although current research is primarily preclinical, including rodent studies on cocaine addiction, anecdotal human reports suggest ketogenic diets may help resolve addictions to substances like cocaine and alcohol. Dr. Msino emphasizes the need for more robust clinical research and collaborative efforts to fully understand and harness this potential. She also touches on the broader implications for food addiction, stress-induced relapse, metabolic psychiatry, and neurological disorders such as epilepsy and autism, where adenosine and metabolic therapies like ketogenic diets may offer therapeutic benefits.
Finally, the discussion includes broader evolutionary and physiological perspectives on adenosine as a stress-response molecule that helps brains adapt and learn, as well as potential non-dietary interventions such as exercise and hot yoga to stimulate adenosine. Dr. Msino calls for increased research and funding to explore adenosine’s unique role in modulating brain function, addiction, and metabolic health.
Highlights
- 🧠 Dopamine drives addictive behaviors but adenosine acts as a natural brake on dopamine’s effects.
- 🥑 Ketogenic diets may increase adenosine by boosting mitochondrial ATP production, influencing addiction pathways.
- 🔬 Current research is mostly preclinical but promising anecdotal evidence exists for ketogenic diets reducing cocaine and alcohol addiction.
- 😴 Adenosine promotes sleep and neuroprotection, linking metabolic health with mental health and addiction recovery.
- 🔄 Addiction, sleep disorders, depression, and metabolic dysfunction often co-occur and may be addressed simultaneously through metabolic therapies.
- 💡 Adenosine also plays a role in epilepsy control and potentially other neurological and psychiatric disorders.
- 🤝 More collaborative research and funding are needed to explore adenosine’s full therapeutic potential in addiction and brain health.
Key Insights
-
🧬 Adenosine-Dopamine Interaction as a Therapeutic Target: Adenosine receptors, particularly the A1 subtype, form heteromers with dopamine receptors, creating a balancing mechanism where increased adenosine activity suppresses dopamine signaling. This molecular interaction can blunt the excessive dopamine surges that underlie addictive behaviors, suggesting that therapies enhancing adenosine could reduce addiction severity and relapse risk. This insight opens new avenues for addiction treatment beyond traditional pharmacotherapy.
-
🥑 Metabolic Health and Addiction Are Deeply Linked: Ketogenic diets enhance mitochondrial function and raise ATP levels, which subsequently increase extracellular adenosine concentrations. This metabolic shift not only supports brain energy demands but also modulates neurotransmitter systems related to addiction and mood regulation. Addressing addiction through metabolic interventions like ketogenic diets could therefore target root causes rather than just symptoms, providing a holistic approach to recovery.
-
🧠 Adenosine’s Multifunctional Role in Brain Health: Beyond addiction, adenosine acts as a neuroprotective agent during metabolic stress, a sleep promoter, and a modulator of epigenetic changes. Its role as a “pan-disease molecule” makes it a promising target for various neurological and psychiatric disorders, including epilepsy, depression, Huntington’s disease, and autism. Enhancing adenosine signaling may confer broad brain health benefits, especially when combined with metabolic therapies.
-
🔄 Stress and Hypoglycemia as Addiction Relapse Triggers: Stress-induced relapse is a major challenge in addiction treatment, and both adenosine signaling and glucose metabolism influence stress responses. Ketogenic diets may stabilize blood sugar levels and reduce stress-related triggers for relapse by modulating adenosine pathways. This dual mechanism highlights the importance of metabolic stability in maintaining long-term sobriety and mental health.
-
🍽️ Translatability to Food and Behavioral Addictions: The mechanisms involving dopamine and adenosine in substance addiction likely extend to non-substance addictions such as food, sugar, and behavioral addictions (e.g., cell phone use, gambling). Since these addictions share dopaminergic reward pathways, metabolic interventions that regulate adenosine could potentially help manage compulsive behaviors across diverse addiction types.
-
🧪 Need for Human Clinical Trials and Interdisciplinary Research: Most existing data on adenosine and ketogenic diet effects on addiction come from animal studies or anecdotal reports. Dr. Msino emphasizes the necessity of well-designed human clinical trials to confirm efficacy and mechanisms. Collaborative efforts among neuroscientists, psychiatrists, nutritionists, and metabolic researchers are critical to advancing this field and creating effective metabolic psychiatry treatments.
-
🏋️ Non-Dietary Ways to Modulate Adenosine: Besides ketogenic diets, physiological interventions such as exercise, hot yoga, acupuncture, and brain stimulation therapies may elevate adenosine levels and improve brain plasticity. These options offer complementary or alternative routes to harness adenosine’s benefits for addiction, mental health, and neuroprotection, broadening therapeutic possibilities.
Conclusion
This interview underscores a groundbreaking paradigm where metabolic therapies, especially ketogenic diets, could revolutionize addiction treatment by modulating adenosine and dopamine pathways. Adenosine’s unique role as a neuroprotective, sleep-promoting, and epigenetic-regulating molecule positions it at the intersection of brain metabolism and addiction neuroscience. While preliminary evidence is promising, especially from animal studies and anecdotal human reports, rigorous clinical research is essential to validate these findings and translate them into practice. The integration of metabolic health into psychiatry could simultaneously address addiction, mental illness, and neurological disorders, offering hope for more effective, multifaceted treatments.
Stefahn Daniel Jasper—a 45-year-old African American truck driver and patient who has transformed his health by adopting a low-carb diet on the road.
Despite long hauls, truck stop temptations, and limited access to healthy food, Stefahn successfully reduced his hemoglobin A1c, improved his liver function, and normalized his urine microalbumin—all while spending most of his life behind the wheel.
Together, we discuss practical tips for low-carb eating on the go, the mindset shifts needed to overcome obstacles, and how drivers across the country can reclaim their health—one mile at a time. This episode is proof that even with a demanding lifestyle, you can take control of your health.
summerizer
Summary
This podcast episode features an in-depth, candid conversation with Stefan Daniel Jasper, a 45-year-old truck driver who has successfully embraced a low-carb lifestyle to manage his type 2 diabetes while living life on the road. Despite the considerable challenges of maintaining a healthy diet amidst constant travel and limited food options, Stefan has transformed his truck into a “rolling sanctuary of health.” He shares practical strategies, such as using an electric skillet powered by the truck’s cigarette lighter and relying on grocery store purchases to prepare nutritious, low-carb meals like eggs, steak, and sausage.
Stefan’s motivation stems from a deep desire to live long for his loved ones and avoid the complications faced by family members and celebrities lost to diabetes. His journey began after confronting dangerously high A1C levels (around 10), which indicated progressive diabetes and the risk of transitioning to type 1. Gradually, he replaced carb-heavy fast foods with protein-and-fat-rich meals, utilizing technology like the Dexcom G6 continuous glucose monitor and carb counting apps to track and manage his blood sugar.
His discipline led to remarkable improvements in key health markers including lowered A1C, normalized urine protein tests (indicating better kidney function), and better liver health, which maintained his energy and alertness on long drives. Stefan emphasizes low-carb substitutes, like keto tortillas and bread, and mindful indulgences with low-impact treats such as sugar-free peanut butter cups and protein shakes. He also discusses practical tips and lifestyle habits, including drinking hot lemon water to aid digestion and hydration, cutting out sugary snacks and condiments like ketchup, and being strategic about alcohol consumption.
Stefan’s story highlights how truck drivers—who often face skepticism about the feasibility of healthy living on the road—can adopt incremental, sustainable changes to profoundly impact their health. His supportive fiancé and family provide additional accountability, and his focus includes not only diet but plans to incorporate more exercise. This episode offers inspiration, practical advice, and a reminder that even those with demanding, unpredictable lifestyles can take control of their health through intentional choices and resourcefulness.
Highlights
- 🚚 Stefan transforms his truck into a “rolling sanctuary” for health with low-carb meal prep.
- 🍳 Uses an electric skillet plugged into the cigarette lighter to cook protein-rich meals on the road.
- 🩺 Dramatic health improvements: A1C lowered from 10 to around 6, improved liver and kidney function.
- 📱 Leverages technology like Dexcom G6 glucose monitor and carb counting apps for real-time tracking.
- 🥩 Advocates replacing bread with keto-friendly wraps and buns to drastically cut carbs.
- 💧 Drinks hot lemon water to aid hydration, digestion, and blood sugar regulation.
- 🧠 Stresses the importance of gradual lifestyle changes and foresight to avoid diabetes distress.
Key Insights
-
🚦 Navigating Health on the Road Requires Creativity and Planning: Stefan’s innovative use of portable cooking equipment and strategic grocery shopping debunks the myth that truck driving and healthy eating are incompatible. This highlights that with some resourcefulness (electric skillet, small refrigerator space, meal prep) healthier choices are accessible even in a highly challenging environment.
-
🥚 Protein and Fat as Stable Fuel for Diabetics: By shifting his diet away from carbohydrate-heavy fast foods to protein and fat (eggs, steak, sausage), Stefan experiences far fewer blood sugar swings and reduced cravings. This reduces the cycle of insulin spikes and sugar crashes, stabilizing energy and decreasing snack dependence, a critical insight for those managing insulin resistance.
-
📊 Continuous Glucose Monitoring Empowers Behavior Change: The use of the Dexcom G6 allows real-time feedback on the immediate impact of foods, drinks, and activities on blood sugar. This transparency motivates adherence and supports informed, data-driven dietary choices, reinforcing the broader value of technology in chronic disease self-management.
-
💡 Small Substitutions Can Have Big Impacts: Swapping out bread for keto tortillas or wraps dramatically lowers carb intake—from nearly 100 grams at a fast food sandwich to under 10 grams—without sacrificing the sensory experience of favorite meals. This demonstrates how nutritional success often hinges on practical, manageable swaps rather than total deprivation.
-
🌿 Hydration and Digestion Play Underrecognized Roles in Blood Sugar Control: Stefan’s incorporation of hot lemon water as a daily routine exemplifies how simple habits can aid digestion and nutrient absorption, while also mitigating false hunger signals often confused with thirst. Such insights emphasize the multidimensional nature of metabolic health beyond just macronutrients.
-
💪 Emotional and Social Supports Are Crucial: Stefan credits his fiancé, family, and the ability to share glucose data for their encouragement and accountability, illustrating how chronic disease management benefits from community and relational support—not just individual willpower.
-
🧠 Mindset and Flexibility Can Sustain Long-Term Change: Stefan’s awareness around conscious indulgences and willingness to “start slow” highlight the psychological components of dietary transformation. His balanced approach allows for occasional treats while maintaining overall glycemic control, providing a realistic model of sustainability rather than perfectionism.
Expanded Analysis and Contextualization
Stefan’s experience removes the false dichotomy often presented between demanding jobs like truck driving and sound health practices. The unique obstacles of life on the road—irregular schedules, fast food availability, cramped quarters—are tackled head-on through adaptability. His investment in small portable cooking tools and meal prepping mirrors successful diabetes interventions in other remote or resource-limited settings, underscoring that infrastructure constraints don’t prohibit health-conscious choices.
The physiological rationale for a low-carb approach is well-articulated: carbohydrates, especially refined and starch-heavy foods, provoke larger insulin responses, which trigger cyclical hypoglycemia and hunger. Stefan’s shift to fat and protein breaks that cycle, stabilizing blood sugar and reducing excessive caloric intake prompted by incessant snacking. This metabolic improvement is validated by his medical labs and clinical markers—a practical demonstration of how nutritional interventions translate to measurable health outcomes.
The benefit of real-time digital health tools—including the Dexcom continuous glucose monitor and carb counting apps—is a major highlight. Seeing one’s glucose values surge or stabilize immediately after eating drastically enhances motivation and self-efficacy. In this sense, technology is not just a monitoring device but a behavioral catalyst, enabling more nuanced understanding of individual variation in food responses and lifestyle factors like sleep and stress.
Notably, the discussion on hydration and lemon water offers a lesser-known but impactful mechanism: proper hydration can reduce false hunger cues, improve digestion, and even accelerate weight management by promoting renal water excretion. Such everyday habits can complement dietary shifts and have additive benefits for metabolic health.
Emotional health and social support emerge as pivotal themes; knowing loved ones are monitoring and encouraging Stefan fosters accountability while reducing the isolation that chronic illness can cause. The open communication stream via sensor-sharing apps exemplifies how modern management can integrate interpersonal ties.
Lastly, the conversation underscores the importance of moderation and flexibility to sustain long-term lifestyle transformations. Stefan’s vacation indulgences and subsequent return to form exhibit resilience rather than rigidity, acknowledging the human element of dietary change and stressing grace over perfection. This balanced mindset prevents burnout and supports ongoing adherence.
In sum, Stefan’s story is a compelling case study in how intentionality, practical innovation, technology use, and supportive relationships can empower individuals—even those in unconventional and challenging professions—to reclaim their health and thrive despite systemic barriers. It is both an instructional blueprint and an inspiring testament to the power of change.
This comprehensive episode will resonate deeply with anyone managing diabetes or metabolic health in demanding contexts, presenting a hopeful, actionable pathway toward better health that harmonizes with life’s realities rather than opposing them.
This is just the abstract:
The study participants comprised 731 Japanese outpatients with type 2 diabetes and no evident cardiovascular disease history. Lifestyle habits, including diet, were assessed with questionnaires at baseline and at years 2 and/or 5, and their mean values were calculated using the average value of lifestyle factors from baseline to the date of onset of an event or the end of follow-up. A multivariable Cox proportional hazards model was used to determine the relationships between each lifestyle habit and the primary endpoint events, comprising cardiovascular events and all-cause mortality.
During the mean follow-up period of 7.5 ± 2.4 years, composite primary endpoint events occurred in 55 participants. Multivariate Cox models showed a significant positive association between the mean proportion of carbohydrate intake and the primary endpoint incidence (hazard ratio = 1.06; 95% CI, 1.02-1.10; P = .005); in addition, the mean total low-carbohydrate diet score, animal low-carbohydrate diet score, and mean proportion of saturated fatty acid intake showed significant inverse associations with the incidence of the primary endpoint.
Our data demonstrated that a higher proportion of carbohydrate intake, particularly with reduced consumption of animal-derived fat/protein, was correlated with an increased risk of cardiovascular disease and all-cause mortality. These data underscore the need to consider dietary components in people with type 2 diabetes.
I'd love to find the full paper, but the normal sites don't have it.

It is frequently claimed that a VLCARB sets the stage for a significant loss of muscle mass as the body recruits amino acids from muscle protein to maintain blood glucose via gluconeogenesis. It is true that animals share the metabolic deficiency of the total (or almost total) inability to convert fatty acids to glucose [18]. Thus, the primary source for a substrate for gluconeogenesis is amino acid, with some help from glycerol from fat tissue triglycerides. However, when the rate of mobilization of fatty acids from fat tissue is accelerated, as, for example, during a VLCARB, the liver produces ketone bodies. The liver cannot utilize ketone bodies and thus, they flow from the liver to extra-hepatic tissues (e.g., brain, muscle) for use as a fuel. Simply stated, ketone body metabolism by the brain displaces glucose utilization and thus spares muscle mass. In other words, the brain derives energy from storage fat during a VLCARB.
https://doi.org/10.1186/1743-7075-3-9 Full paper
Tom DeLauer claims Ozempic and keto may share eerily similar effects… but is that really true? Dr. Eric Westman reacts to Tom’s breakdown of GLP-1s vs. low-carb diets. Are you just suppressing appetite — or rewiring your metabolism? What’s the real cost of “easy weight loss”? From visceral fat loss to ketone production, we explore the surprising overlaps and hidden dangers. Could pairing medication with diet unlock a better result — or are we just medicating bad habits?
summerizer
Summary
In this in-depth video, Dr. Eric Westman analyzes and compares the effects and mechanisms of GLP-1 receptor agonists, such as Ozempic, with ketogenic (keto) and low-carbohydrate diets, particularly in the context of weight loss and metabolic health. He provides a critical review of studies, including those highlighted by keto community influencer Tom Dauer, to assess how these pharmaceutical agents and dietary protocols similarly reduce hunger, promote fat loss, and impact metabolism, while clarifying crucial differences between them.
Dr. Westman emphasizes that both GLP-1 medications and keto diets suppress appetite naturally, leading to fewer calories consumed without active calorie counting. Ozempic and related drugs mimic gut hormones responsible for satiety, causing significant calorie deficits, which often result in substantial fat loss, especially in visceral fat—a dangerous fat stored around internal organs linked to inflammation and health risks. At the same time, ketogenic diets induce metabolic ketosis by carb restriction, shifting the body into fat-burning mode, which also naturally decreases hunger.
While GLP-1 agonists tend to produce more rapid and pronounced calorie reductions (about 725 calories/day resulting in roughly 5 kg fat loss over study duration), keto diets also lead to meaningful calorie deficits (160-200 calories/day) and fat loss. However, keto diets confer additional benefits by improving metabolic flexibility, preserving muscle mass through ketones and hormone modulation, and fostering a "cleaner" metabolic state by reducing carbohydrate oxidation.
A key theme is the difference in metabolic processes during weight loss with medication versus diet alone. GLP-1 medications suppress hunger pharmacologically but do not necessarily change the metabolic substrate preference; users may continue oxidizing carbohydrates depending on their diet. In contrast, a ketogenic diet induces a metabolic shift that preferentially burns fat and produces ketones, which have muscle-sparing and metabolic regulatory effects.
Dr. Westman also discusses challenges, such as side effects and sustainability. Weight loss medications often cause low energy or nausea and may not encourage lasting lifestyle changes, leading to potential weight regain when stopping the drug. Keto diets require adaptation and withdrawal from carbs but build behavioral habits that may better support maintenance. Importantly, combining GLP-1 therapy with a low-carb or keto diet could maximize benefits, but also increase side effects, necessitating clinical supervision.
Dr. Westman underscores that until randomized controlled trials directly comparing keto diets with GLP-1 therapies exist, definitive conclusions are limited. Nevertheless, he advocates for using these tools strategically—weight loss drugs can help patients "get over the hump," especially with significant visceral fat reduction, but diet remains fundamental for sustainable metabolic health. He encourages viewing GLP-1 agonists as adjuncts, not replacements, to effective dietary and lifestyle interventions.
Highlights
- 🧬 Both GLP-1 drugs and keto diets suppress appetite naturally, leading to effortless calorie reduction.
- 🔥 Ozempic users experience about a 725-calorie daily deficit and significant fat loss, including visceral fat.
- 🥩 Keto diets promote metabolic ketosis and fat burning without the medication, preserving muscle and improving metabolic health.
- ⚖️ Weight loss through medication and diet differ metabolically: medication users may still burn carbs, keto dieters shift fully to fat oxidation.
- 💊 Combining GLP-1 drugs with low-carb/keto can enhance fat loss but increase side effects; clinical oversight is essential.
- 🏋️ Muscle preservation is better on low-carb/keto due to ketones and hormone effects than with medication alone.
- 🔄 Sustainability challenges exist with medication-only approaches without behavioral change, risking weight regain.
Key Insights
-
🌱 Appetite Suppression via Different Mechanisms but Similar Outcomes: Both GLP-1 receptor agonists and ketogenic diets reduce hunger without explicit calorie restriction, yet through distinct physiological pathways. GLP-1 mimics gut satiety hormones pharmacologically, directly signaling fullness, whereas keto diets induce metabolic changes causing natural appetite regulation via fat oxidation and ketone production. This convergence means both approaches can effectively reduce calorie intake unconsciously, supporting weight loss without deliberate dieting, a critical factor in long-term adherence.
-
🥑 Metabolic Differences Influence Fat Loss Quality and Muscle Preservation: Weight loss medications suppress appetite but do not inherently change substrate oxidation patterns; if the diet remains high in carbs, the body continues burning glucose. In contrast, keto diets shift metabolism toward fat and ketones as primary fuel, facilitating preservation of lean muscle through hormonal pathways like increased growth hormone and ketone-mediated muscle sparing. This muscle retention during weight loss is crucial for metabolic health, physical functionality, and prevention of weight rebound.
-
🔬 Visceral Fat Loss is Rapid with GLP-1 but Sustainability is Key: Studies show that GLP-1 drugs like Ozempic can reduce visceral fat by up to 25%, an impressive reduction with significant potential to reduce inflammation and chronic disease risk. However, Dr. Westman warns that losing visceral fat via drugs alone without changing eating habits often results in weight regain once medication is discontinued. This highlights the importance of coupling pharmacologic treatment with sustainable lifestyle changes to maintain health benefits.
-
⚡ Energy Levels and Exercise Capacity May Be Impacted by GLP-1 Therapy: The medication-induced satiety and nausea can cause low energy, mirroring the post-large meal lethargy experience. This makes exercising, especially intense forms like high-intensity training (HIT), challenging while on the medication. In contrast, people on a keto diet may maintain better energy levels for resistance or aerobic training, aiding muscle preservation and metabolic health. Therefore, exercise prescription and lifestyle coaching are pivotal adjuncts regardless of treatment.
-
🧩 Combining GLP-1 Agonists with Low-Carb/Keto Strategies Offers Synergy but Requires Caution: Clinically, combining the appetite suppressant medication with a low carbohydrate or ketogenic diet may potentiate fat loss effects and muscle preservation benefits, but carries risks of increased side effects such as gastrointestinal distress or excessive energy deficit. This combination demands delivery by clinicians knowledgeable in both pharmacology and nutrition, underscoring the need for personalized medicine and close patient monitoring.
-
🔄 Behavioral Modification and Environmental Control are Critical for Lasting Success: Weight loss shots create a window of opportunity where appetite is reduced, making it easier to modify food environments and behaviors—such as clearing high-carb junk foods from home—to support long-term adherence once medication ends. This integration of medication-induced appetite suppression with behavioral and environmental strategies offers a pathway to sustainable weight management, something neither approach achieves in isolation.
-
🎯 Need for Direct Comparative Clinical Trials to Guide Evidence-Based Practice: There is a notable lack of randomized controlled trials directly comparing keto or low-carb diets to GLP-1 therapies, limiting clinical guidance. Dr. Westman calls for rigorous trials with active treatment arms for both diet and medication to understand differential effects on weight, fat distribution, metabolism, muscle preservation, side effects, and sustainability. Such data could inform personalized approaches and cost-effective treatment choices in obesity care beyond pharmaceutical marketing influence.
Conclusion
Dr. Westman’s analysis presents a nuanced view that both GLP-1 receptor agonists and ketogenic diets are powerful tools for appetite suppression and fat loss but operate through different metabolic mechanisms with unique advantages and limitations. While medications provide a rapid pathway to fat loss, especially visceral fat, keto diets offer cleaner metabolic adaptation, muscle preservation, and potential for behavioral change leading to durable outcomes.
Clinicians and patients must weigh these differences thoughtfully, considering side effects, energy levels, sustainability, and lifestyle preferences. Combining pharmacologic and dietary interventions may yield the best results in some cases but requires expert supervision due to possible amplified adverse effects.
In the evolving landscape of obesity treatment, Dr. Westman advocates for evidence-based, integrated approaches that transcend silos between drugs and diets, urging further well-designed research to optimize therapy selection and long-term success.
CGMs from aliexpress are $20 USD for two weeks of blood glucose monitoring. I think as part of everyone's normal health monitoring they should slap on a CGM and just see how they are doing, maybe once a year or two.
Especially if someone is having problems, weight issues, sticking to a diet... the immediate visual feedback of seeing blood glucose in real time is a game changer and makes sticking to a plan much more effective.
There are a bunch of issues you can see with just glucose monitoring
- Diabetes (heh)
- Poor glycemic control (insulin resistance)
- Stress
- Sleep issues
- Hypoglycemia (insulin resistance again)
- "snack" frequency
- fake "health" foods that spike glucose
Someone with a "normal" hba1c can have really spikey glucose control which means their quickly approaching full insulin resistance, and the CGM would show that years before the hba1c creeps up

Dr Erin Louise Bellamy founded Integrative Ketogenic Research and Therapies which uses principles of Metabolic Psychiatry to provide remote, highly personalized 1:1 Metabolic Therapy for both psychiatric conditions and overall metabolic health.
Dr. Erin Bellamy has a PhD in Psychology, specializing in Ketogenic Diets & Depression from the University of East London. She also has an MSc in Psychiatric Research from the Institute of Psychiatry at King’s College London. She is a Chartered Psychologist, an Associate Fellow of the British Psychological Society and an accredited member of the Society of Metabolic Health Practitioners.
In this episode, Drs. Brian and Erin talk about…
(00:00) Intro
(01:36) How Dr. Erin became interested in Metabolic Psychiatry
(05:38) Ketogenic diets and psychiatric conditions
(15:39) Fasting and mental clarity
(18:12) The areas in which clinical psychology is deficient in helping patients
(23:46) Adverse childhood events, PTSD, and metabolic health
(28:24) Binge eating, stress, and support groups
(40:00) Food addiction and ketosis
(43:59) Schizophrenia, autism, and ketosis
(01:00:46) Outro/plugs
summerizer
Summary
This episode of the Low Carb MD podcast features Dr. Erin Bellamy, a psychologist and metabolic health practitioner (MHP), who shares her compelling journey into metabolic psychiatry—the emerging field that addresses mental health through metabolic and nutritional interventions such as ketogenic diets. Dr. Bellamy recounts her early experiences working on psychiatric inpatient wards and her research path, which revealed striking historic and modern evidence showing profound mental health improvements linked to low-carbohydrate and ketogenic therapies.
The conversation highlights the strong interconnection between metabolic health and mental health, emphasizing how metabolic dysregulation, particularly in conditions like diabetes and schizophrenia, can directly impact mood, cognition, and psychiatric symptoms. Dr. Bellamy stresses the importance of a multidisciplinary approach, combining nutrition, sleep, light exposure, exercise, and psychological support to build resilience against mental illness.
The podcast also addresses systemic challenges in mental health care such as medication-centric models, long wait times for psychiatric care, and the lack of holistic lifestyle integration. Dr. Bellamy explains her group programs designed to educate and support people with various psychiatric diagnoses through ketogenic metabolic therapy, fostering community and sustained lifestyle change. Throughout, hope and empowerment surface as central themes, underscoring that with appropriate metabolic care and social support, even treatment-resistant symptoms can improve dramatically.
Highlights
- 🧠 Metabolic health is a foundational pillar for improving mental health conditions such as schizophrenia, bipolar disorder, and depression.
- 🍳 Ketogenic diets historically and currently show promising results in alleviating severe psychiatric symptoms.
- ⏳ There is a disturbing research gap between early studies (1960s) and modern psychiatry overlooking nutrition’s role in mental health.
- 👥 Group support and community involvement significantly increase adherence and success in metabolic psychiatry interventions.
- 🚀 Multidisciplinary collaboration including psychologists, psychiatrists, and metabolic health practitioners is critical for integrated care.
- 🔄 Metabolic psychiatry offers hope for treatment-resistant mental illness by addressing root metabolic dysfunctions.
- 🌱 A holistic pyramid approach with nutrition as the base, supplemented by sleep, stress management, exercise, and social connection is vital. Key Insights
🧬 The metabolic basis of mental illness is historically recognized yet underappreciated: Dr. Bellamy points to early research from as far back as 1930s and a pivotal 1965 study showing ketogenic diets improving schizophrenia symptoms. This suggests a biological underpinning of mental disorders linked to metabolic processes, which modern psychiatry has largely sidelined in favor of drug-centric interventions.
🔄 Metabolic dysregulation precedes and exacerbates psychiatric symptoms: The discussion reveals that poor blood sugar control and insulin resistance can precipitate depression and anxiety rather than these mental illnesses being purely psychological or behavioral in origin. This shifts the treatment paradigm toward addressing metabolic imbalances as causal factors.
🤝 Holistic, multi-layered care improves outcomes: Dr. Bellamy’s “metabolic pyramid” model prioritizes nutrition as the foundation, with layers including sleep optimization, light exposure, exercise, stress reduction, and social connection. This comprehensive strategy recognizes that sustainable mental health improvements require addressing environmental, lifestyle, and biochemical factors simultaneously.
💬 Social and clinical support enhances adherence: Ketogenic and metabolic therapies demand significant lifestyle changes, which are difficult without structured support. The podcast underscores the critical role of group programs, peer accountability, and integration into multidisciplinary teams to maintain motivation and long-term success, especially in complex psychiatric populations.
🔍 Current mental health systems inadequately address metabolic health: Patients face long waits for psychiatric care focused narrowly on medications with debilitating side effects that worsen metabolic health. Psychologists are positioned to bridge the gap but are often disconnected from nutritional interventions. A reframing toward metabolic psychiatry could transform treatment protocols.
🌿 Hope and patient empowerment are therapeutic: Offering patients a tangible, active role in managing their health through ketogenic metabolic therapy fosters agency and reduces feelings of helplessness common in chronic mental illness. The ability to control symptoms through diet and lifestyle has profound psychological benefits beyond physiology alone.
⚖️ Flexibility and balance are key: Successful programs encourage realistic planning, allowing occasional social indulgences without guilt, emphasizing control and balance rather than strict deprivation. This practical approach supports mental wellbeing and reduces relapse driven by shame or all-or-nothing mindsets.
This episode illuminates how revisiting and integrating metabolic science into mental health care offers groundbreaking potential for improving lives devastated by psychiatric illness. Dr. Bellamy’s experience and research-based optimism call for a paradigm shift to holistic, metabolism-centered psychiatry supported by community and clinical collaboration.
What really happens when you stop eating carbs? In this intense video, Dr. Eric Westman responds to bold claims from Dr. Paul Saladino — once a leading carnivore voice — about the dark side of keto: cortisol spikes, thyroid dysfunction, and falling testosterone. Are these concerns valid or just fear-based interpretations of short-term studies? With clinical insight and years of experience, Dr. Westman untangles fact from hype. Stick around for his final verdict — the real story may surprise you.
summerizer
Summary
In this video, Dr. Eric Westman critically examines the claims made by an influencer physician, Dr. Saladino, who moved from an enthusiastic carnivore and ketogenic diet advocate to a critic of low-carb and ketogenic diets. Dr. Westman explores the physiological impacts of carbohydrate restriction, particularly focusing on stress hormones such as cortisol, epinephrine, glucagon, and thyroid hormone changes. He underscores that while ketogenic diets induce elevated stress hormones initially, this may normalize over time with adaptation. More importantly, he emphasizes the distinction between the classical ketogenic diet used for treating epilepsy—often severe and medically supervised—and the more flexible ketogenic diets employed for metabolic health, diabetes reversal, and obesity treatment.
Dr. Westman points out that many of the cited studies—often short-term and involving small or specific populations such as epileptic children—are not directly transferable to the broader adult population using ketogenic diets for health improvement. He highlights that blood markers like thyroid hormones and cortisol may fluctuate on ketogenic diets, but these changes do not necessarily reflect negative health outcomes or cellular dysfunction. Instead, certain physiological adaptations occur as part of the body’s metabolic recalibration.
He also discusses how carbohydrate intake positively affects exercise recovery, cortisol reduction, testosterone levels, and immune function, acknowledging that these benefits may be significant for athletes or those engaging in intensive training. However, he challenges the notion that these findings universally condemn ketogenic diets, especially for non-athlete populations. Dr. Westman stresses individualized approaches to nutrition and the importance of interpreting biochemical markers in the appropriate clinical context rather than relying solely on blood values or short-term studies.
Ultimately, Dr. Westman calls for more nuanced, long-term research and cautions against broad, fear-based generalizations about ketogenic diets. He encourages those interested to monitor their own health markers with professional guidance and recognizes that multiple dietary paths can support health and vitality.
Highlights
- 🔬 Elevated cortisol and glucagon are physiological responses to low-carb diets but may normalize with adaptation.
- 🩺 Short-term ketogenic diet studies, especially in epilepsy patients, may not apply to adult keto dieters for metabolic health.
- ⚖️ Blood thyroid hormone variations on keto don’t always equal clinical hypothyroidism or poor metabolic function.
- 🏋️ Carbohydrate intake improves exercise recovery, testosterone, and reduces cortisol after intensive workouts.
- 🔄 Keto adaptation can take months; early adverse markers may reflect transition rather than harm.
- 📊 Different ketogenic diets vary widely; findings on one variation shouldn’t be generalized to all.
- 🧬 Individual metabolic responses require personalized monitoring rather than fear-based blanket dietary advice.
Key Insights
-
🧪 Adaptive Stress Hormone Response: The increase in cortisol, epinephrine, and especially glucagon during carbohydrate restriction is a well-documented physiological mechanism to maintain glucose homeostasis. While cortisol and adrenaline levels may diminish over time with metabolic adaptation, glucagon remains elevated on low carb diets as a primary regulator of blood sugar. This highlights that elevated stress hormones do not necessarily indicate pathological stress but rather a fundamental metabolic shift. Awareness of this is crucial to avoid misclassification of normal metabolic adaptation as a harmful stress state.
-
⏳ Short-Term vs. Long-Term Evidence: Many negative conclusions about ketogenic diets stem from short-term studies (e.g., three to six weeks) or highly specialized populations such as children with intractable epilepsy. These early time points often capture the “keto flu” or transition period before full adaptation. Long-term studies and clinical experience suggest many of these initial negative markers (bone remodeling markers, thyroid hormones) stabilize once adaptation occurs. Thus, premature conclusions about keto’s safety and efficacy based on transient data are unreliable.
-
🩸 Thyroid Hormone Complexity in Keto: Keto diets may reduce circulating T3 levels, but interpreting these blood values requires clinical context. Decreased circulating thyroid hormones during weight loss, regardless of diet type, can reflect a normal adaptation to reduce metabolic rate rather than true thyroid dysfunction. Moreover, symptoms and cellular hormone activity need to be assessed, not just serum levels. Overreliance on blood tests without clinical correlation can lead to misdiagnosis and unnecessary alarm.
-
⚡ Carbohydrates and Exercise Performance: Carbohydrate consumption improves key exercise-related outcomes such as cortisol attenuation, immune function, and free testosterone. For athletes or highly active individuals, carbs can be a valuable performance and recovery tool. However, since ketogenic dieters typically experience a metabolic shift prioritizing fat utilization, their “normal” ranges and performance baselines differ markedly. Therefore, benefits of carbs in exercise might not translate into a clear detriment in non-athletic keto followers.
-
🔬 Metabolic Diversity of Keto Diets: There is no monolithic “keto diet.” Variants range from extreme ketogenic protocols used in seizure management to more liberal carbohydrate restriction plans aimed at diabetes reversal or weight loss. Studies and critiques often conflate these, leading to misinterpretation. Evaluations of keto must specify the diet type, population, and medical context. This diversity necessitates cautious generalizations about keto’s benefits or risks.
-
👩⚕️ Importance of Individualized Monitoring: Rather than accepting broad, universal statements about the dangers or benefits of ketogenic diets, Dr. Westman advocates for personalized health monitoring. Key labs—thyroid panels, cortisol, glucose, lipid profiles—should be interpreted by experienced clinicians who consider symptoms and context. This approach recognizes metabolic individuality and the fact that biochemical markers have nuanced meaning depending on dietary pattern and adaptation status.
-
📚 Critical Evaluation of Online Influence: Dr. Westman reminds viewers of the importance of scrutinizing influencer information, particularly from medical professionals with self-reported anecdotal experiences that may not generalize. Professional training, rigorous clinical practice, and comprehensive understanding of physiology and biochemistry matter in interpreting diet-related claims. Blindly adopting one person’s experience as universal truth risks overlooking the complex mosaic of human metabolism.
This video thus offers a balanced, evidence-informed perspective on ketogenic diets, advocating for reasoned analysis, patience during adaptation, and personalized nutritional strategies rather than blanket condemnations or endorsements.
For fat loss the single most important thing you can do is reduce your insulin levels, which means keeping your sugar and carbohydrate intake to a minimum. If your not ready to give up carbohydrates entirely, try to keep all your carbs to one meal and the rest of your day protein and fat only.
If you have the budget for it I highly, highly, highly recommend getting a CGM (continuous glucose monitor) - It gives you immediate feedback on your blood glucose levels all day (insulin follows glucose). Keep the glucose line flat and you will lose amazing amounts of fat.
Have a look at the carbohydrate insulin model of obesity TLDR - Don't worry about CICO, food restriction, even exercise - the only thing you have to do is keep your insulin levels flat and carbohydrate levels low.
Don't lose weight to get healthy. Get healthy to lose weight.
The intuitive explanation:
Insulin is a super hormone -it drives anabolism (gaining fat), and prevents adipose catabolism (burning fat). When insulin levels are high, you cannot burn fat. Insulin also drives glucose out of the blood into adipose tissue (this is why you can't burn fat when insulin is high) - elevated glucose levels are really damaging to the body- it is a priority to get them out of the blood.
Every time you eat carbohydrates your blood glucose goes up, and then your insulin levels go up... hitting the pause button on any fat loss until you burn through all that glucose. If your goal is to burn fat, you need to keep those insulin levels low as much as possible - which means limit your carbohydrate consumption as much as possible.
That's it, the big secret to fat loss - keep insulin low by limiting carbohydrates to a small (or zero) window every day.
Are ketogenic diets dangerous? What about nutrient deficiencies, gout, gut health, keto rash, bone density loss, or kidney stones?
In this video, registered dietitian and ketogenic therapy expert Beth Zupec-Kania, RDN, CD, shares insights from over 30 years of clinical experience to address the most common concerns and misconceptions about ketogenic therapies.
From vitamin and mineral intake to gallbladder issues, sleep disruptions, leg cramps, keto flu, and more, this interview covers it all.
Beth also explains how ketogenic therapy can be adapted for various lifestyles, preferences, and health conditions, and offers practical tips for managing social situations, emotional transitions, and athletic performance while following a well-formulated ketogenic diet.
In this interview, you’ll learn:
- Why many concerns stem from outdated pediatric protocols
- How to safely supplement and avoid nutrient deficiencies
- What to know about the microbiome, bowel habits, and fiber intake
- How to prevent keto flu, leg cramps, and other common keto side effects
- When to be cautious with medications that impact bone or kidney health
- How keto may support those with eating disorders—not cause them
Whether you're just starting out or considering ketogenic therapy for epilepsy, type 2 diabetes, mental health, weight loss, or another condition, this video will help ease your mind of many of the concerns around ketogenic dieting.
Whether you're new to metabolic therapies or exploring ketogenic strategies for conditions like epilepsy, type 2 diabetes, serious mental illness, weight loss, or another condition, this video addresses common concerns and offers clarity on how a well-formulated ketogenic diet can be a powerful, science-backed option worth considering.
Expert Featured: Beth Zupec-Kania, RDN, CD
summerizer
Summary
The video transcript provides an in-depth exploration of the ketogenic diet, focusing on its medical applications, common misconceptions, physiological effects, and strategies to safely transition into and maintain ketosis. The discussion differentiates nutritional ketosis, achieved safely in controlled ketogenic diets, from ketoacidosis, a dangerous condition mainly occurring in type 1 diabetes due to insufficient insulin. The expert, dietitian Beth Zupca, shares her extensive clinical experience, particularly with pediatric epilepsy patients, highlighting the evolution of ketogenic therapies from rigid, classic protocols to more flexible, nutrient-rich approaches.
Key physiological challenges during the transition to ketosis such as leg cramps and the “keto flu” are explained as consequences of electrolyte imbalances and fluid shifts. Solutions like increasing salt and mineral intake, hydration, and electrolyte supplementation are recommended to alleviate symptoms. The transcript stresses individualized diet plans, addressing the specific needs of different groups, including athletes and those with treatment-resistant eating disorders. Emotional adaptation, including overcoming the psychological loss of familiar comfort foods, is underlined, promoting creative substitutes and open communication with family and social circles to mitigate social isolation.
The transcript also clarifies common misconceptions: the ketogenic diet is not a license for unrestrained fat and bacon consumption but a tailored nutrition plan adaptable to various preferences. Concerns regarding bone density, microbiome health, and uric acid fluctuations are contextualized and often debunked as myths or transient effects. The speaker concludes by encouraging education through trusted resources and a commitment to advancing public understanding of the ketogenic diet’s health benefits, safety considerations, and therapeutic potential.
Highlights
- 🔬 Nutritional ketosis is safe and distinct from ketoacidosis, which is mostly a diabetic complication.
- 🥗 Modern ketogenic diets are flexible and nutrient-dense, not restrictive or deficient.
- 💧 Electrolyte imbalance during keto transition causes leg cramps and “keto flu,” manageable with hydration and salt.
- 🏋️♂️ Ketogenic diet plans should be individualized, especially for athletes or those with special medical conditions.
- 🍳 The ketogenic diet is not merely a “bacon and butter” diet; it includes diverse food options tailored to preferences.
- 🧠 Emotional and social adaptation is vital—finding alternatives to comfort foods and seeking support eases transition.
- 📚 Reliable education and clear communication help dispel myths and promote safe, effective ketogenic diets.
Key Insights
🔥 Distinguishing Nutritional Ketosis from Ketoacidosis: Nutritional ketosis is a controlled metabolic state achieved safely under medical supervision, primarily through ketogenic diets, whereas ketoacidosis involves dangerously high ketone levels and acidosis due to insulin deficiency in type 1 diabetes. This differentiation is crucial to debunk common fears about ketogenic diets and underscores their therapeutic potential when carefully monitored.
💧 Electrolyte Management is Crucial During Transition: The onset of ketogenic diets prompts renal excretion of sodium, potassium, chloride, and magnesium, contributing to symptoms like leg cramps and the “keto flu.” Proactive supplementation with salt and minerals alongside increased hydration is essential to mitigate these adaptation symptoms and maintain comfort and adherence.
🥑 Evolving Ketogenic Therapies Enhance Nutrient Adequacy: Classic ketogenic diets were once perceived as restrictive and nutrient-poor; however, contemporary protocols have evolved to include diverse, nutrient-rich foods and individualized supplementation strategies that address concerns about nutrient deficiencies, bone health, and microbiome balance. This evolution supports long-term sustainability and broadens applicability beyond pediatric epilepsy.
🏃♀️ Individualized Approaches Optimize Exercise and Metabolic Health Outcomes: Athletes and active individuals on keto may require adjusted calorie and fat intake to support endurance and performance. The ketogenic diet’s flexibility allows tailoring to distinct metabolic demands and lifestyle factors, enhancing its therapeutic and wellness benefits.
🧠 Addressing Psychological and Social Challenges Fosters Diet Adherence: Transitioning to keto involves emotional adjustments as individuals cope with the loss of familiar comfort foods and social eating norms. Encouraging alternative snacks and open communication with family and friends helps reduce feelings of social isolation, promoting psychological well-being and sustainable lifestyle changes.
⚖️ Debunking Myths Strengthens Public Trust: Misconceptions such as the ketogenic diet promoting eating disorders or being an excuse for excessive fatty food consumption undermine its legitimacy. Presenting evidence-based clarifications that keto is adaptable, health-focused, and supportive of diverse needs encourages wider acceptance and safer utilization.
🌐 Education and Trusted Resources Empower Users: Limited social media presence paired with curated educational resources stresses the importance of seeking credible guidance. Empowering people with accurate, nuanced information ensures safer adoption, better adherence, and improved health outcomes from ketogenic diets.
This comprehensive analysis underscores that ketogenic diets, when properly managed, offer safe, flexible, and effective nutritional strategies with significant therapeutic and health benefits across diverse populations.
In this episode of the KetoPro Podcast, Richard Smith interviews Dr. Dan Plews, youtube.com/@EndureIQ a renowned sports scientist and coach, who shares his extensive knowledge on low-carb diets and their impact on athletic performance. Dr. Plews discusses his academic background, his transition from high-carb to low-carb diets, and the benefits of ketosis for endurance athletes. He emphasizes the importance of individualized nutrition, the role of protein, and the need for adaptation periods in optimizing performance. The conversation also touches on real-life success stories, the influence of the sports industry on dietary guidelines, and the future of training in high rocks.
Takeaways
Dr. Dan Plews has a diverse background in sports science and coaching. Low-carb diets can significantly improve endurance performance. Ketosis is a natural metabolic state that can benefit athletes. Individualized nutrition is crucial for optimal performance. Protein should be prioritized in an athlete's diet. Carbohydrate intake should be tailored to the athlete's needs. Adaptation periods are essential for transitioning to low-carb diets. The sports industry influences dietary recommendations for athletes. Real-life success stories demonstrate the effectiveness of low-carb diets. High rocks training offers a new avenue for athletes transitioning from traditional endurance sports.
summerizer
Right Fuel, Right Time... Low carb for Athletic Performance?
In this episode of the Keto Pro podcast, Richard Smith hosts Dr. Dan PL to discuss the impact of low carbohydrate diets on athletic performance. Dr. PL shares insights from his extensive experience as an academic and sport scientist, focusing on the adaptation of athletes to low carb diets and the importance of macronutrient manipulation for performance optimization. They explore the misconceptions surrounding carbohydrate intake for endurance athletes and debate the effectiveness of lower carb versus high carb diets, emphasizing individualized nutrition plans based on performance needs.
Key Points
Introduction of guests and backgrounds
Richard Smith welcomes Dr. Dan PL, an expert in sports science and a coach based in New Zealand. Dan discusses his extensive background, including his research on heart rate variability, coaching roles, and personal achievements as an athlete, specifically in triathlon.
Challenges with high carbohydrate diets
Dr. PL and Richard discuss the prevalent belief among athletes that higher carbohydrate intake is necessary for performance. Dr. PL highlights how athletes become dependent on carbohydrates and may struggle to perform without them, drawing parallels to addiction.
Experience with lower carbohydrate diets
Dr. PL shares his personal journey of transitioning to a low carbohydrate diet, highlighting improvements in his performance and adaptation. He underscores the significance of individualized nutrition, suggesting that all athletes can benefit from experimenting with their diets.
Misconceptions in the athletic community
The conversation delves into why many athletes resist the idea of low carb diets. Dr. PL notes that misconceptions abound, as traditional beliefs often overshadow emerging research suggesting benefits of lower carbohydrate intake.
Adaptation period for low carb diets
They discuss the adaptation period required for athletes who switch to low carb diets, indicating that it can take several weeks for the body to adjust and improve performance.
Scientific evidence versus anecdotal experience
Richard and Dr. PL debate how anecdotal successes of elite athletes with high carbohydrate diets can mislead average athletes. They stress the importance of using scientific evidence as a guide for nutritional practices.
Role of protein and macronutrient balance
Dr. PL emphasizes the importance of protein in athlete diets and discusses finding a balance between carbohydrates, fats, and proteins to optimize performance without relying excessively on carbohydrates.
Future of athletic nutrition
They conclude with thoughts on the evolution of nutritional guidelines in sports, urging a shift towards individualized approaches that honor both health and performance needs.
Does keto really prevent colon cancer? Dr. Eric Westman reacts to a viral clip featuring Dr. Shawn Baker and Dr. Layne Norton, who debate a study claiming the ketogenic diet suppresses colorectal cancer via gut microbiome changes. Are mouse studies enough? What about fiber and red meat? This reaction cuts through hype, bias, and overclaims to help you understand the science without the spin.
summerizer
Does This Diet Really Fight Cancer?!
Dr. Eric Westman reacts to a viral discussion about the ketogenic diet's potential role in preventing colon cancer. He critically analyzes a mouse study presented by Shawn Baker and discusses the need for human-based research, emphasizes the Warburg effect, and critiques the use of epidemiological studies in nutrition debates, particularly concerning red meat and fiber intake.
Key Points
Debate Over Keto and Colon Cancer
Dr. Westman addresses a social media post regarding a study suggesting that the ketogenic diet may help suppress colon cancer. He clarifies that while the study was done on mice, human studies are necessary for concrete conclusions.
Historical Context of Keto and Cancer
The discussion references Otto Warburg's early 20th-century observation that cancer cells thrive on glucose, providing a rationale for the ketogenic diet's potential benefits against cancer by limiting glucose availability.
Importance of Study Design
Westman criticizes those who dismiss epidemiological studies while selectively citing them when convenient. He points out the flaws in the mouse study, emphasizing the need for human studies to validate claims.
Fiber's Role in Colon Cancer
The video discusses conflicting views on the relevance of fiber in cancer prevention, with Westman supporting the traditional view of fiber's benefits, while addressing Baker's claims against its necessity.
Caution Against Overselling Unverified Research
Westman urges caution in promoting claims about keto and cancer prevention that are not yet backed by substantial human research, emphasizing the importance of scientific evidence in dietary recommendations.
Is nutrition research getting the support it needs to inform public health policy?
Despite the rise in chronic diseases related to lifestyle factors like diet, nutrition research only receives $2.2 billion of the $30 billion NIH budget.
At first glance, this may seem like a lot of money, but its utilization is spread thin, and, as Dr. David Ludwig and Gary Taubes highlight in this interview, it’s primarily used to fund misleading short term trials that confirm existing nutrition biases.
However, if we want to actually address the chronic disease epidemic, we must increase the resources allocated to nutrition research AND the quality of that research.
In this video, journalist Gary Taubes and Harvard endocrinologist Dr. David Ludwig expose the core problems in today’s most cited nutrition studies and offer a bold new path forward.
In this conversation, you’ll learn:
Why short-term feeding studies can’t tell us much about chronic disease How confirmation bias shapes which nutrition studies get funded, published, and accepted by the medical community and policy makers The major flaws in NIH-funded research comparing low-carb vs. low-fat diets Why the focus on ultra-processed foods is only part of the solution How we could design better long-term studies that actually help people get healthier
It’s time to question the status quo and demand better utilization of research funds to inform public health policy in a way that can impactfully improve the health of our population.
Resources Mentioned: Studies
- doi.org/10.1136/bmj-2024-082963
- doi.org/10.1101/2023.10.03.23296501
- jamanetwork.com/journals/jama/fullarticle/2673150
- nejm.org/doi/full/10.1056/NEJMoa1212914
- doi.org/10.1016/j.cmet.2019.05.008
Short-term diet trials are designed to fail
- statnews.com/2025/04/22/nutrition-precision-health-short-term-diet-trials-chronic-disease-food
Gary's Substack Article
- uncertaintyprinciples.substack.com/p/nih-has-a-nutrition-problem-part
summerizer
The Truth About Nutrition Science: Is The Government Getting it Wrong?
This video features a discussion on the shortcomings of nutrition research and its impact on public health policy, particularly concerning the rising rates of obesity and diabetes. Experts Gary Taubes and Dr. David Ludwig analyze the challenges in nutrition science, the effectiveness of current studies, and propose how to improve research methods moving forward. They emphasize the need for long-term, well-funded clinical trials that explore the low-carb and processed food diets, questioning the biases in interpreting nutrition studies.
Key Points
Confusion in Nutrition Science
Many people feel lost about nutrition due to conflicting studies and beliefs. The current state of nutrition science has not effectively addressed chronic diseases like diabetes and obesity.
Funding and Research Quality
Nutrition research is severely underfunded compared to pharmaceutical studies, which leads to insufficient data on effective dietary guidelines and the underlying causes of obesity and diabetes.
Issues with Current Studies
Many of the prominent studies suffer from design flaws and biases, particularly studies that confirm pre-existing beliefs within the nutrition community, leading to misleading conclusions.
Need for Better Studies
A call for longer, well-supported clinical trials focusing on the carbohydrate insulin model and low-carb diets. These studies should take into account real-world food environments and patient adherence.
Ultrarocessed Foods Debate
While ultrarocessed foods are commonly viewed as unhealthy, the discussion around their impact lacks thorough scientific examination, and more nuanced, detailed studies are needed.
Challenges for Professionals
Health professionals struggle to recommend diets that have not been broadly validated through rigorous, long-term trials, which limits their ability to provide effective dietary guidance.
Opportunity for Change in Research
With new leadership in nutrition research agencies like the NIH, there may be an opportunity to reshape the focus and funding of future nutrition studies.
AI and Nutrition Precision
The potential for using AI in personalized nutrition may complicate the situation further. Experts stress the importance of foundational studies before tailoring diets to individual needs.
Just in your life, how many people's lives have you improved? Have you found keto to be a good tool for your friends and family?
Food noise is a term that makes sense to many people. Food noise is a great way to describe the unhealthy way many people think about food, and what they consider to really be food. But, food noise is not the problem, it is only the symptom of a much bigger problem.
Some people can combat and defeat food noise on their own, and some need help...
summerizer
Dr. Ken Barry explains the concept of 'food noise', which is the incessant craving and preoccupation with unhealthy foods. He argues that food noise is a symptom of addiction to sugar and ultra-processed foods rather than a new medical condition. Barry critiques the pharmaceutical industry's response to this phenomenon, proposing that the solution lies not in medications but in dietary changes, particularly eliminating ultra-processed foods and focusing on whole foods, like beef, butter, bacon, and eggs, to break the addiction cycle.
Key Points
Definition of Food Noise
Food noise refers to the persistent cravings and thoughts about food, especially unhealthy options, that individuals experience shortly after eating. Dr. Barry emphasizes that food noise is not a new medical term but rather a symptom of deeper issues related to food addiction.
Marketing of Food Noise
The term 'food noise' gained popularity recently, coinciding with the approval of drugs like Ozempic. Dr. Barry criticizes the introduction of this term as a marketing strategy to promote pharmaceuticals that treat the symptoms rather than address the root causes, such as sugar and carbohydrate addiction.
Nature of Cravings
Barry points out that people generally experience food noise regarding sugary, ultra-processed foods, rather than whole, nutritious foods. He highlights the correlation between these cravings and an addiction to high sugar and carb diets.
Food Industry Manipulation
The video discusses how food manufacturers design their products to exploit human biology, using flavors and ingredients that trigger hunger and suppress satiety, leading consumers to overeat.
Pharmaceutical Solutions vs True Solutions
Dr. Barry warns against relying on pharmaceutical interventions like Ozempic for managing food noise, advocating instead for dietary changes to replace unhealthy eating habits.
Carnivore Challenge
Barry introduces a 90-day diet challenge of only eating beef, butter, bacon, and eggs, designed to help individuals break free from their sugar and food addiction. The challenge aims to reset hunger and satiety signals in the body.
Long-Term Health Considerations
The speaker emphasizes the risks of long-term pharmaceutical usage for managing hunger and satiety, highlighting the lack of safety research and suggesting that individuals may become unwitting participants in pharmaceutical experiments.
Encouragement for Dietary Change
He urges viewers to consider the dietary changes he proposes not only for personal health improvement but also to assist others suffering from food noise, stressing the large percentage of adults affected by ultra-processed food addiction.
Fewer than 1% of patients with type 1 diabetes achieve normal glycemic control (glycated hemoglobin [HbA1c] < 5.7%/ < 39 mmol/mol). Additionally, exogenous insulin administration often causes “iatrogenic hyperinsulinemia,” leading to whole-body insulin resistance and increased risk of cardiovascular complications. We present data on the clinical efficacy and safety of a long-term (10-year) ketogenic diet (≤50 g carbohydrates/day) therapy in a patient with type 1 diabetes. The use of a ketogenic diet resulted in successful glycemic control, assessed by HbA1c (5.5%; 36.6 mmol/mol), continuous glucose monitoring median glucose (98 mg/dL; 5.4 mmol/L), and glucose time-in-range of 70 to 180 mg/dL (90%) without acute glycemic complications. In conjunction, there was a** 43% decrease in daily insulin requirements**. Low-density lipoprotein cholesterol increased, whereas small-dense low-density lipoprotein was in the normal range (<90 nmol/L). No adverse effects were observed on thyroid function, kidney function, or bone mineral density. This case report demonstrates that a long-term ketogenic diet in a person with type 1 diabetes has considerable therapeutic benefits.
Full Text: https://doi.org/10.1210/jcemcr/luae102
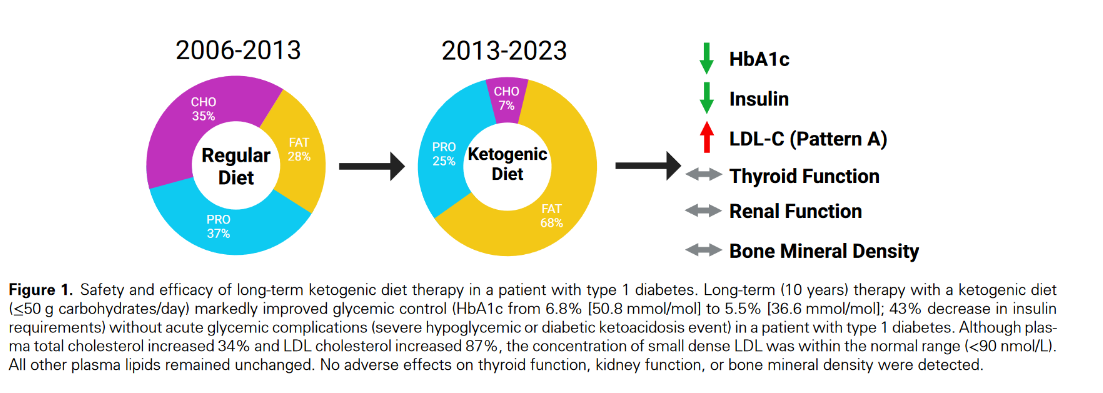
Colorectal cancer (CRC) patients have been shown to possess an altered gut microbiome. Diet is a well-established modulator of the microbiome, and thus, dietary interventions might have a beneficial effect on CRC. An attenuating effect of the ketogenic diet (KD) on CRC cell growth has been previously observed, however the role of the gut microbiome in driving this effect remains unknown. Here, we describe a reduced colonic tumor burden upon KD consumption in a CRC mouse model with a humanized microbiome. Importantly, we demonstrate a causal relationship through microbiome transplantation into germ-free mice, whereby alterations in the gut microbiota were maintained in the absence of continued selective pressure from the KD. Specifically, we identify a shift toward bacterial species that produce stearic acid in ketogenic conditions, whereas consumers were depleted, resulting in elevated levels of free stearate in the gut lumen. This microbial product demonstrates tumor-suppressing properties by inducing apoptosis in cancer cells and decreasing colonic Th17 immune cell populations. Taken together, the beneficial effects of the KD are mediated through alterations in the gut microbiome, including, among others, increased stearic acid production, which in turn significantly reduces intestinal tumor growth.
Full Paper https://doi.org/10.1038/s41467-025-56678-0

Having just suffered a major carving attack yesterday (I won), this video touches on the very important topics of controlling urges. It's a super short 4m video.
How To Stop My Food Cravings For Good Are your cravings controlling you? In this video, Dr. Tony Hampton breaks down the real root cause of cravings—and it’s not just about willpower. Learn how ultra-processed foods hijack your brain's reward system, how dopamine drives the craving cycle, and how to finally rewire your brain for long-term control.
Using stories, science, and simple tools, Dr. Hampton helps you understand the dopamine-craving loop, the roles of stress, sleep, hormones, and gut health, and the power of nutrition—especially low-carb and carnivore diets—to quiet food noise and restore peace of mind.
You’ll also hear about Lisa, a patient whose nightly ice cream habit felt impossible to break—until she discovered what was really going on inside her brain.
summerizer
How To Stop My Food Cravings For Good
Dr. Tony Hampton discusses how to effectively manage and overcome food cravings by understanding their root causes, particularly in the brain, and provides strategies for rewiring mindset around food. He emphasizes the impact of diet, sleep, stress hormones, and food marketing in creating cravings, and suggests practical steps to break the cycle of addiction to sugar and processed foods.
Key Points
Cravings are a brain issue, not just stomach hunger.
Dr. Hampton explains that cravings are driven by brain circuits rather than merely physical hunger. The brain has been conditioned to seek out rewarding foods, leading to behaviors that resemble addiction.
Stop the cycle by removing triggers.
He advises removing food triggers from the home environment. If unwanted food isn't available, it's less likely to be consumed, thereby helping to break the cycle of cravings.
Focus on nourishing foods.
Emphasizing the importance of consuming protein, healthy fats, and whole foods, Dr. Hampton recommends low carb and carnivore diets as effective strategies to stabilize blood sugar levels and reduce cravings.
Resist cravings to weaken brain circuits.
By resisting cravings and replacing them with healthier habits, individuals can weaken the neural pathways that reinforce cravings, ultimately leading to a reduction in their frequency.
Dopamine fast to reset taste sensitivity.
He introduces the concept of a dopamine fast— abstaining from sugar and processed foods for three days—which can help recalibrate taste buds and reduce cravings for hyper-palatable foods.
Avoid moderation traps.
Dr. Hampton cautions against the idea of moderating unhealthy foods, arguing that such a tactic can perpetuate the craving. Instead, consistent effort is required to break free from addiction.
Encourage self-compassion and resetting.
If someone slips up, they should avoid self-judgment and instead focus on resetting their habits. Understanding the root causes helps combat guilt and regain control over food choices.
Very-low-calorie diets (VLCDs) are used to treat obesity, often in a non-clinical setting, and the typical formulation of a minimum of 50 g carbohydrates daily can induce a mild dietary ketosis. This clinically benign state is sometimes confused with the non-metabolically adapted state of ketoacidosis, and this misunderstanding may lead to the rejection of VLCDs as a suitable obesity treatment. This paper summarises and discusses the difference between physiological ketosis and pathological ketoacidosis, the benefits of ketosis-inducing weight-loss regimen such as VLCDs and why ketoacidosis should never be the diagnosis in a non-type 1 diabetic on a carbohydrate-restricted diet.
Paper https://doi.org/10.1111/j.1467-3010.2011.01916.x
Full Paper on scihub

Dr. Eric Westman reacts to Dr. Sten Ekberg’s breakdown of the top 10 foods RFK Jr. is aiming to ban. From artificial dyes to sugary cereals and seed oils, are these policies really about health or missing the bigger picture?
summerizer
RFK Jr Just Banned These 10 Foods!
In this video, Dr. Eric Westman discusses Dr. Sten Ekberg's analysis of RFK Jr.'s proposed bans on ten specific foods and drinks, focusing on their health impacts and the implications for dietary practices. Westman critiques the effectiveness of banning certain additives while suggesting a broader approach to improving dietary health through reduced carbohydrate consumption and healthier food options.
Key Points
Artificial Dyes Ban
RFK Jr. targets artificial dyes commonly used in processed foods, which have been linked to health issues and banned in many countries. Dr. Westman argues that the focus should shift to the unhealthy foods containing these dyes rather than merely eliminating the dyes themselves.
SNAP Program Restrictions
Kennedy seeks to eliminate sugary and ultraprocessed foods from the Supplemental Nutritional Assistance Program (SNAP), advocating for healthier options in federal programs. Dr. Westman supports this, stating that access to healthier foods could reduce health disparities in low-income populations.
High Fructose Corn Syrup
RFK Jr. aims to reduce the use of high fructose corn syrup in government programs. Westman points out that it metabolically behaves similarly to regular sugar, questioning whether removing one while allowing the other will make a significant difference.
Seed Oils
Kennedy wants to limit seed oils, known for promoting inflammation. Westman acknowledges the concern but suggests that further evidence is needed to justify drastic changes, emphasizing that diet high in carbohydrates is a more pressing issue.
Ultraprocessed Foods
The video discusses the disadvantages of ultraprocessed foods like pizza and sugary cereals in schools. Westman agrees with removing these items, highlighting the necessity for healthier alternatives that also consider carbohydrate content.
Artificial Sweeteners
Kennedy proposes a ban on artificial sweeteners, which Dr. Westman believes should remain available to help individuals cut sugar while still enjoying sweetness. He contends that there is insufficient evidence to deem them harmful.
Grass Loophole Reform
Kennedy's call for reform relates to food additives deemed 'generally recognized as safe.' Westman stresses the need for careful evaluation of substances in our food rather than blanket approvals based on outdated criteria.
Raw Milk Advocacy
Kennedy supports raw milk for its nutritional benefits, but Westman is cautious, suggesting a thorough examination of the associated risks and benefits.
Sugary Cereals and Yogurts
The removal of sugary cereals marketed as healthy is also discussed. Westman believes that real food alternatives should replace these highly sugary processed options.
Processed Meats
Westman critiques RFK Jr.'s focus on restricting processed meats due to sodium nitrite concerns, arguing their relevance is less significant compared to overall carbohydrate intake.
This video is family friendly. The title is referring to a high fat diet making your big pants baggy, as you lose weight.
How I lost 145 lbs in 14 months, cured my acid reflux, lost my joint pain, and lowered my triglycerides, by eating butter and other healthy fats.
Did you know Butter can make your pants fall off?
Neither did I until I started eating butter and cream and bacon and eggs and Fatty cuts of chicken cooked in good old fashioned lard.
I lost 145 pounds in 14 months and was amazed to see eating Butter made my size 54 pants fall off.
I’m not kidding when I say Butter Makes Your Pants Fall Off
I’m living proof that it worked for me and know it will work for you.
Hello, my name is Bob, I’m fifty years old, I’m not a diet guru, I’m just an average working class guy and I know my story sounds crazy, but I hope you’ll hear me out if you’re fat and sick and hurting, I hope you’ll give me a few minutes of your time, because I believe my story could really change your life.
summerizer
Butter Makes Your Pants Fall Off
Bob Briggs shares his personal journey of losing 145 pounds over 14 months on a high fat, low carb diet where he embraced foods like butter, cream, bacon, and eggs. He explains how insulin resistance contributes to weight gain and suggests that eating fat helps control appetite while promoting weight loss. He challenges conventional diet beliefs and advocates for a diet free from sugary foods, which he considers toxic for those prone to obesity.
Key Points
Personal Transformation
Bob Briggs details his personal weight loss journey, explaining that he lost 145 pounds in 14 months by embracing a high-fat, low-carb diet. His story serves to inspire those who might feel hopeless about their weight.
Insulin Resistance
He introduces the concept of insulin resistance, which affects individuals with a belly fat problem, highlighting how this condition inhibits fat burning and leads to weight gain. He believes that understanding insulin's role is crucial to combating obesity.
Dietary Changes
Briggs emphasizes the importance of reducing carbohydrate intake, specifically sugars, while increasing fat consumption. He argues that consuming fat, contrary to popular belief, actually helps with weight loss and appetite control.
Health Benefits of High-Fat Diet
He shares his health improvements, stating that his cholesterol levels and overall health markers became better as a result of his dietary changes, debunking the myths surrounding fat consumption and heart health.
Challenging Diet Norms
Briggs questions traditional weight-loss wisdom that equates calories with body weight. He asserts that the quality of food consumed, particularly the types of carbohydrates, plays a larger role in weight gain than caloric intake alone.
Long-Term Lifestyle Changes
He concludes with the notion that adopting a low-carb, high-fat lifestyle can lead to sustained weight loss and improved health, encouraging viewers to reconsider their dietary choices for a healthier and happier life.